This is a very common complaint in the paediatric setting and often is a diagnostic challenge due to an unreliable history from the child who is also often uncooperative with the physical examination. ‘
There are a wide variety of possible causes. It could be due to:
- Bone Conditions
- Intra-articular Conditions
- Neuromuscular Conditions
- Soft-tissue conditions
- Spinal Conditions
- or even, Intra-abdominal causes
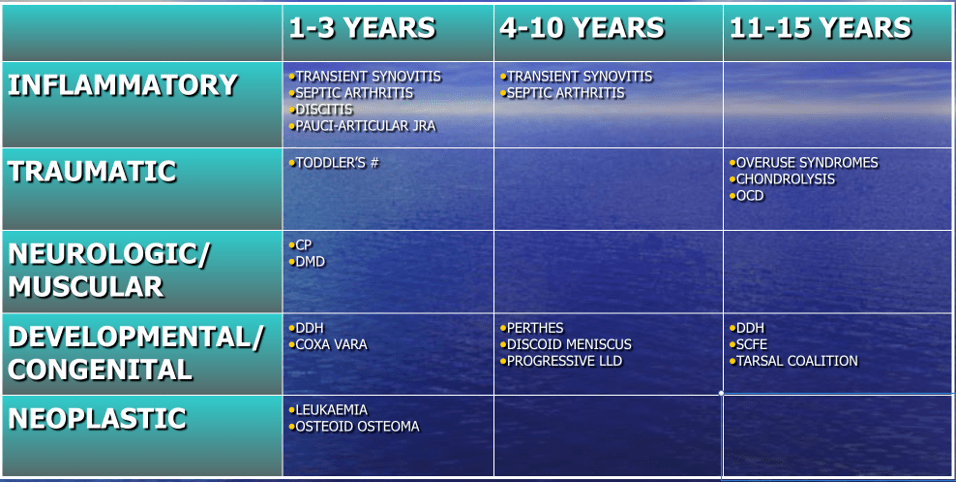
We find it prudent to look at the more common orthopaedic causes from an age-group perspective as different age-groups have different predilections.
1) Transient Synovitis
- More commonly seen in ages 3-8, although it is seen from ages 1 all the way to 10.
- The cause is uncertain and it may sometimes be preceded by a viral infection.
- Child may or may not exhibit a fever along with hip pain and a limp.
- Treated symptomatically.
- Important to rule out SEPTIC ARTHRITIS.
2) Septic Arthritis
- Children are more prone to this because of sluggish blood flow in the vessels of the growing bones.
- The child presents with fever, painful joint and a limp as well as an exquisitely painful range of movement.
- Investigations need to be performed and once ascertained, surgical drainage is a necessity.
- This is a surgical emergency as it can cause joint destruction.
3) Diskitis or Disc Space Infection
- Children are more prone to this because of the way the blood vessels supply the disc from the bone.
- It affects the lumbar spine most commonly.
- The child may exhibit a limp, have a loss of appetite, abdominal pain and sometimes run a fever.
- Radiological and blood investigations are necessary and will help to guide treatment.
4) Toddler’s Fracture
- This is the result of a twisting (torsional) injury to the leg.
- The history might be unremarkable indeed, but the child will have a limp and may be unable to bear weight.
- Initial radiological investigations may look normal or show a hairline crack. A repeated one may be necessary after a few days.
- Treatment is immobilisation with a cast.
5) Cerebral Palsy
- The child presents differently in this case.
- There could be a delay in the commencement of walking and may have always had an abnormal gait.
- There could have been a significant peri-natal (birthing) history.
- There is poor balance, and the degree of limp is dependent on the severity of the condition.
6) DDH (Developmental Dysplasia of Hip)
- In Singapore, as we routinely screen the infant’s hips, this is usually diagnosed at birth.
- This is a condition where the “ball and socket” joint of the hip does not properly form in babies and young children. This results in abnormal development leading to subluxation or even dislocation of the hip.
- Hence it is important to diagnose this early so the hip can be reduced into the correct position to allow for normal development.
7) SCFE (Slipped Capital Femoral Epiphysis)
- This is a condition which affects the adolescent and involves a slip at the growth plate of the hip so that the neck of the thigh bone translates while the head stays in the joint.
- The presentation may not necessarily be acute. However, it should be examined as soon as possible, as certain types require early surgical intervention to prevent growth deformities.
- Simple radiological investigations are usually all that is required to clinch the diagnosis.
8) Perthe’s disease
- This is a condition in which the blood supply to the head of the hip bone is compromised.
- It tends to affect boys more and may first present with a painless limp, with pain setting in as it progresses. This is then associated with a limitation in the range of movement of the hip.
- Early radiological investigations may be normal. A high clinical suspicion would warrant further forms of imaging.
- The aim is to control symptoms, restore range of motion and achieve containment of the hip joint.
- Hence early diagnosis is important
9) Discoid Lateral Meniscus
- Can present from ages 3-12 or later.
- There is no history of trauma, but the child demonstrates a painful limp with clicking and swelling over the outside of the knee, and worsened with activity.
- An MRI is required for the diagnosis.
- Surgery may be required to treat the symptoms.
10) Limb Length Discrepancy
- There is a difference in the length of the lower limbs leading to an abnormal gait. This worsens as growth and the discrepancy progresses.
- There are many causes for this and can be due to congenital (present at birth), to paralytic (neuromuscular), to growth plate disorders.
- It is important to delineate the cause so that early management can be instituted.
- There is a 2cm discrepancy in 2/3 of the normal population.
- Hence treatment may only be indicated in cases in which the discrepancy exceeds 2cm.
- Radiological and laboratory investigations can be done.
- Surgical management options may involve closing of the growth plates early, to shortening or lengthening of the bones.
11) Overuse Syndromes
- These occur in the rapid phase of growth in the adolescent in concert with increased participation of sporting activities.
- OSD (Osgood Schlatter’s Disease), Jumper’s knee are examples.
- Physical examination +/- radiological investigations will help to clinch the diagnosis and allow the start of treatment.
- This usually involves rest with some physiotherapy as required
12) Osteochondritis dissecans/ Osteochondral Lesion
- The joint cartilage and underlying bone is affected leading to pain.
- It occurs mostly in the knee and ankle but can affect the elbow as well.
- It can be hereditary, due to vascular problems or traumatic.
- The cartilage and underlying bone is injured, and as the insult progresses, it starts to detach.
- As the disease progresses the joint congruity is lost and this can predispose to earlier onset of osteoarthritis.
- Treatment involves off-loading the area affected. Surgery may be indicated to allow healing of the is affected.
13) Tarsal Coalition
- This is usually a congenital condition (present at birth), in which the symptoms begin to manifest at adolescence as the bones mature.
- There is a bridge between the bones of the feet, leading to pain or abnormal movement leading to symptoms.
- Treatment depends on the severity of the symptoms. Not all cases would require surgical intervention as some can manage the symptoms with rest and change or modification of footwear. Intractable cases would benefit from surgery freeing up the joints to move in the normal articulation.
Looking For A Reliable Paediatric Orthopaedic Orthopaedic Specialist?
Fast Medical Attention, Transparent Fees
Make an appointment for comprehensive care for your paediatric orthopaedic problems!
