What is Limb Length Discrepancy (LLD)?
Small Limb Length Discrepancies of up to 2cm are common and are present in the normal, asymptomatic population.
Patients respond differently in their tolerance and compensation of their LLD. Children tend to do so better than adults.
However, it is not just a cosmetic issue, as it can have functional implications. A short leg gait increases energy expenditure, overloads certain other joints leading to early arthritic changes and can cause back pain.
What Causes Leg Length Discrepancy?
There are many possible causes for this. It may be a congenital disorder (present from birth) such as DDH, PFFD, hemihypertrophy; Neurological; a consequence of Trauma; Infection; Inflammatory cause or even due to Tumours/ Dysplasia.
Hence, it is important to rule out some of them, or treat them if need be, before concentrating on the treatment of the LLD.
How Is Leg Length Discrepancy Diagnosed?
LLD of < 2cm can usually be left alone, or prescribed a shoe raise/ insert. LLD > 2cm would require treatment. Therefore it is important to ascertain this.
Examination of the patient involves evaluation of the range of motion as well as the resting position of the patient’s back, hip, knee and ankle joints.
Clinical measurement of the lower limbs is also important and there are several ways to do so, whether it is the use of the measuring tape to measure between bony/anatomical landmarks, wooden blocks placed under the shorter limb to square the pelvis, or a simple screen test known as the Galeazzi Sign.


The microdose CT scan is a very useful investigation. It is less susceptible to error and can account for angular deformity.
Once the LLD is ascertained, the next step is to assess how the discrepancy is likely to progress over time.
There are several ways to calculate this and the calculation also depends on the cause and course. The LLD usually follows an upward linear slope in most of the cases. It should be noted that these predictions are only a guide, as they are based on statistical analysis and calculations, and can never be 100% accurate.
They are most accurately predicted after a series of measurements are obtained over a period of time, preferably from ages 4-10, prior to growth spurt.

How Is Leg Length Discrepancy Treated?
Management of the LLD depends on the size or predicted size of the discrepancy, effect on the patient and their joints. In general, discrepancies <2cm are left alone or prescribed inserts/ shoe raise.
Discrepancies 2-5cm may benefit from the shortening of the longer limb (via bone cuts), or early fusion of the growth plate. These procedures are more predictable than lengthening and are associated with fewer complications.
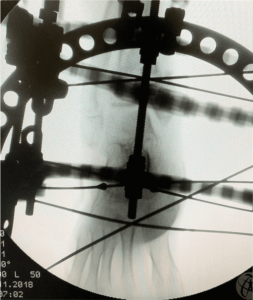
Discrepancies >5cm may require lengthening +/- shortening of the longer limb. This can be achieved via the use of an external ring fixator, or internal intramedullary lengthening nails.
These procedures are more technically demanding and the outcome is not quite as predictable. Although more acceptable aesthetically-wise, they are associated with more complications such as pin-tract infection, muscle, joint and nerve problems.
Thus, the treatment of LLD must be titrated to the conditions and needs of the patient.
Looking For A Reliable Paediatric Orthopaedic Orthopaedic Specialist?
Fast Medical Attention, Transparent Fees
Make an appointment for comprehensive care for your paediatric orthopaedic problems!
